When too little leads to too much
If skin cells lack a particular factor, skin complaints like psoriasis can develop. This is what ETH Zurich biologists have demonstrated in a mouse model, which can easily be applied to humans.
The Serum Response Factor (SRF) protein is well known in cell and development biology. As a so-called transcription factor, it regulates the reading of genetic information by binding to the so-called promoter region of genes.
SRF plays a key role in the development of different organs and tissues. It is an important cog in the regulation of cell division and differentiation, cell migration and cell death. Nevertheless, whether the protein also plays a role in adults’ skin cells remained unknown until recently.
Cell biologists from Sabine Werner’s team at ETH Zurich have taken a big step forward in this respect and can now accredit the factor with yet another crucial function. The study was just published in the Journal of Clinical Investigation.
Without sufficient SRF, skin becomes diseased
In normal, healthy skin, the cells in the upper layer of skin (epidermal keratinocytes) produce relatively large amounts of SRF. This maintains the skin’s equilibrium. However, if there is an absence of SRF for whatever reason (due to the deletion of the corresponding gene locus “srf”, for example), lab mice develop symptoms reminiscent of psoriasis in humans. Just like psoriasis patients, “srf” knockout mice developed flaky, inflamed patches on their backs, paws and tails. In these areas, the skin cells had divided excessively and were no longer able to develop normally.
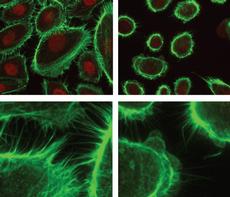
The researchers were able to demonstrate that the skeleton of the skin cells is disturbed and destroyed as a direct result of the SRF deficiency. The cells lose contact with their neighbors and the matrix that surrounds them. Consequently, the outer layer of skin loses its compact layering. Fissures form, which enables water to evaporate more easily and the skin dries out more quickly, thus making the intermediate spaces more susceptible to foreign bodies and bacteria. This in turn triggers an inflammatory reaction that induces the skin cells to divide and impairs their differentiation.
Psoriasis patients lack SRF almost entirely
Interestingly, the ETH-Zurich researchers have now discovered that the affected skin in psoriasis patients almost lacks the SRF protein entirely. Together with the results of the mouse tests, this suggests that the loss of SRF is involved in the development of the common skin disease. Like the mice, psoriasis patients develop red, inflamed patches that constantly shed squames – the necrotic skin cells. The patients thus become partially disfigured and suffer from severe itching. Ointments offer some relief, restoring the protective and barrier function of the skin and, in more severe cases, anti-inflammatory substances. The renowned spa treatment in the mineral-rich water of the Dead Sea can also alleviate the effects of the disease, but not cure it.
Trigger still unknown
The researchers still do not know which factor(s) cause(s) the down-regulation of SRF. This is a key issue which Werner’s team is set to address next. The suspects include other proteins, such as cytokines or other transcription factors. Moreover, we still do not know whether and which triggers from the environment contribute to to the down-regulation of SRF.
For a long time, the school of thought was that abnormalities in the immune system trigger psoriasis. Today, however, the research is also looking for defects in the epidermis that could be genetic or even environmental. “In the case of psoriasis, it is not always the immune system that is the trigger, but often a defect in the keratinocytes,” explains Sabine Werner.







READER COMMENTS